Blog

- Gustavo Lopes, MD
The Latest in Weight Loss Surgery: Advancements, Options, and Considerations

- Jonathan Turkish, MD
- Women's Health
Proactively Curbing Risk Factors, Wellness OB-GYN Care, Can Help Reduce Rise in Endometrial Cancer
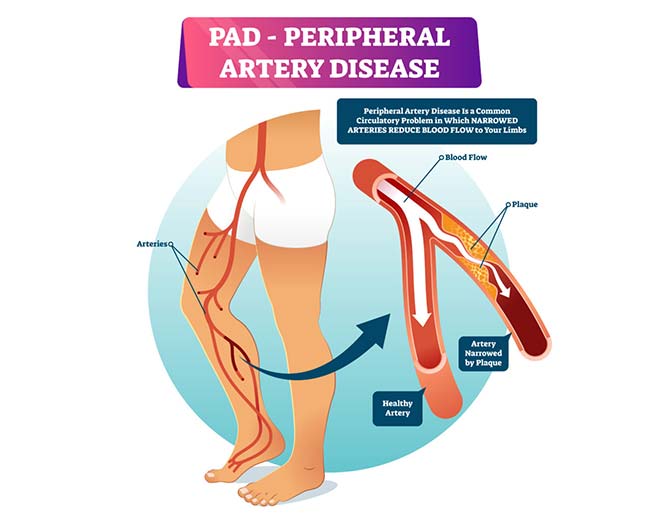
- Cardiovascular
September is Peripheral Arterial Disease (PAD) Awareness Month

- Orthopedics
Get Moving Away From Arthritic Pain!

- Orthopedics
Just as a tire on a car wears down over time, so can the hip joint

- Ali Malek
- Neurology
Sidelined Podcast - Ep. 4 | Transient Ischemic Attacks

- Neurology
Sidelined Podcast - Ep. 3 | Stroke, Cerebral Aneurysm and Brain Hemorrhage

- Orthopedics
Sidelined Podcast - Ep. 1 | Hip Injuries

- General Surgery
Skin Safety Tips for the Summer Sun
- Primary Care
Is it the common cold or the flu?
- Cardiology
Keeping your heart on beat. AFib treatment options.

- Orthopedics
Diagnostic Options in Your Hands

- Orthopedics
Sports Injuries: Fractures and Contusions

- Cardiovascular
After a Stroke: What Caregivers Should Know

- Neurology
The Migraine Spectrum

- Cardiology
Exciting New Treatment Approaches for Atrial Fibrillation
- Orthopedics
Common Questions about Platelet Rich Plasma

- Ali Malek
- Neurology
Stroke: A Threat to Everyone?

- Cardiology
Atrial Fibrillation is not a “One Size Fits All” Disease

- Cardiovascular
After a Stroke: Proper Diet and Nutrition
- Cardiovascular
May-Thurner Syndrome and the Potential for Blood Clots

- Cardiovascular
Surgery Isn’t Your Only Option: Conservative Treatments for Vein Disorders
- Cardiovascular
Help Manage Carotid Artery Disease with Lifestyle Changes

- Cardiology
Broken-Heart Syndrome

- Cardiovascular
Why You Should Choose a Vascular Surgeon for Varicose Vein Treatment.

- Cardiovascular
Everyday Strategies For Preventing Blood Clots
- Cardiovascular
Is Your Weight Affecting Your Veins?

- Cardiovascular
How Smoking Affects Your Vascular System: Know the Risks
- General Surgery
Pancreatic Cancer: What to Know

- Neurology
Epilepsy and Seizures

- Cardiovascular
The Fall and Winter Are The Best Times To Get Your Veins Fixed

- Neurology
Tourette Syndrome: What Is It, Symptoms, Diagnosis & Treatments

- Neurology
Stroke: Despite the Statistics

- Orthopedics
Don’t Be A Pain In The Hip!
- Neurology
Promising New Migraine Research

- General Surgery
Learning from Melanoma – My Personal Story

- Orthopedics
I broke my clavicle - now what?

- Neurology
Parkinson’s Disease: The Need for a Comprehensive Approach
- Colorectal
Colorectal Cancer: Treatment & Prevention

- Endocrinology
Thyroid Cancer: Don't Forget to Check Your Neck

- Orthopedics
Tennis Injuries

- Orthopedics
ACL Tears

- Orthopedics
Treat the Patient, not the MRI

- Orthopedics
Heat Illness and Hydration

- Community
Welcome to the Palm Beach Health Network Physician Groups Blog!

